Affect | Risk Factor | Impact | Silent Heart Attacks | Damage Blood Vessels and Nerves | Symptoms |Heart Failure Treatment | Managing Diabetes and Cardiovascular Health
Diabetes and cardiovascular disease (CVD) are two of the most pressing health issues facing individuals worldwide. With diabetes affecting millions globally and CVD being a leading cause of death, understanding the intricate relationship between these conditions is crucial for effective management and prevention.
This blog delves into how diabetes impacts heart health, the signs to watch for, and the best strategies to manage these intertwined conditions.
Relationship Between Diabetes and Heart Disease
Diabetes and heart disease are closely linked through several mechanisms. High blood sugar levels lead to the formation of arterial plaque and damage to blood vessel linings, increasing the risk of atherosclerosis, heart attacks, and strokes.
Diabetes also contributes to high blood pressure, abnormal lipid levels, and chronic inflammation, all of which exacerbate cardiovascular risk.
Additionally, insulin resistance and autonomic neuropathy further elevate the risk of heart disease. Managing diabetes effectively is essential for reducing these cardiovascular risks and maintaining heart health.
How does Diabetes Affect the Cardiovascular System
Diabetes, particularly type 2 diabetes, is a significant risk factor for diabetes cardiovascular disease. High blood sugar levels associated with diabetes can lead to damage in blood vessels and nerves, which in turn increases the risk of heart disease.
When blood sugar is poorly managed, it can cause inflammation and damage to blood vessel walls, leading to conditions such astype 2 diabetes cardiovascular disease.
Is Diabetes a Risk Factor for Cardiovascular Disease?
Can diabetes cause cardiovascular disease? Yes, diabetes is indeed a risk factor for cardiovascular disease. People with diabetes have a higher risk of developing heart-related issues due to the detrimental effects of high blood glucose on the cardiovascular system. This connection is particularly strong in type 2 diabetes, where prolonged exposure to elevated glucose levels can lead to more severe cardiovascular complications.
The Impact of Diabetes on Heart Health
Diabetes and heart health are totally connected to each other. Diabetes effect on heart health in several ways. Diabetes increased risk of heart disease by elevating blood sugar levels that can lead to:
- Increased Risk of diabetes coronary artery disease (CAD): Diabetes accelerates the process of atherosclerosis (hardening and narrowing of the arteries), which can lead to CAD.
- Diabetes and Heart Failure: High blood sugar levels can impair the heart’s ability to pump blood effectively, leading to heart failure.
- Diabetes and heart rate: Some studies suggest that diabetes can affect heart rate. Individuals with diabetes might experience variations in heart rate, which can be a sign of underlying cardiovascular issues.
- Normal heart rate for type 2 diabetes: For individuals with type 2 diabetes, the normal range for heart rate is generally similar to that for the general population. The typical resting heart rate for adults, regardless of diabetes status, ranges from about 60 to 100 beats per minute (bpm). Factors like physical fitness, stress, medications, and overall health can influence this range.
- Low heart rate and diabetes: A low heart rate, or bradycardia, can be influenced by various factors, and its connection to diabetes is an interesting topic. Diabetes, particularly when poorly controlled, can affect the autonomic nervous system, which regulates heart rate. This can sometimes lead to bradycardia.
- Additionally, certain medications used to manage diabetes or its complications might influence heart rate.
- It’s also worth considering that bradycardia in someone with diabetes might not always be directly related to the diabetes itself. Other factors such as physical fitness, age, medication side effects, or underlying heart conditions could play a role.
- Type 1 diabetes fast heart rate: A fast heart rate, or tachycardia, in someone with type 1 diabetes can arise from several factors, including:
- Blood Sugar Levels: Fluctuations in blood glucose levels can affect heart rate. For example, both hyperglycemia (high blood sugar) and hypoglycemia (low blood sugar) can cause tachycardia as the body responds to these imbalances.
- Autonomic Neuropathy: Type 1 diabetes can lead to diabetic autonomic neuropathy, which affects the autonomic nervous system responsible for regulating heart rate and other involuntary functions. This can result in an abnormal heart rate response.
- Stress or Anxiety: Managing diabetes can be stressful, and anxiety or emotional stress can increase heart rate.
- Medication Side Effects: Some medications used to manage diabetes or related conditions can influence heart rate. For instance, certain insulin formulations or other drugs might have side effects that affect the cardiovascular system.
Diabetes and Silent Heart Attacks
One of the more insidious issues related to diabetes is the phenomenon of silent heart attacks. These heart attacks occur without the typical symptoms, making them harder to detect. People with diabetes may not experience the usual chest pain or discomfort associated with a heart attack. Instead, symptoms can be more subtle or mistaken for other conditions.
Why do Diabetics get Silent Heart Attacks?
Diabetics are at a higher risk of experiencing silent heart attacks, also known as asymptomatic myocardial infarctions, for several reasons:
- Autonomic Neuropathy: Diabetes, especially when poorly controlled, can lead to autonomic neuropathy, which affects the autonomic nervous system that regulates involuntary functions like heart rate and blood pressure.
- Reduced Pain Sensation: The nerve damage associated with diabetes may reduce the sensation of pain. This means that the classic symptoms of a heart attack, such as chest pain or discomfort, may not be felt as intensely or might not be recognized at all.
- Chronic Disease Impact: Diabetes can cause general wear and tear on the cardiovascular system over time.
- Vascular Damage: Diabetes accelerates atherosclerosis (the buildup of plaque in the arteries), leading to more subtle or gradual heart attacks. The gradual progression might lead to less pronounced symptoms or even none at all.
- Increased Risk of Heart Disease: People with diabetes often have multiple risk factors for heart disease, including high blood pressure, high cholesterol, and obesity. This can make heart attacks more common but less symptomatic.
- Misinterpretation of Symptoms: Individuals with diabetes may attribute symptoms such as fatigue, nausea, or shortness of breath to other diabetes-related issues rather than recognizing them as signs of a heart attack.
Because silent heart attacks may not present with clear symptoms, they can often go undetected until they cause significant damage or complications. Therefore, it’s crucial for people with diabetes to regularly monitor their cardiovascular health.
How does Diabetes Damage Blood Vessels and Nerves
In summary, diabetes damages blood vessels and nerves through chronic high blood sugar levels, leading to the formation of harmful AGEs, increased oxidative stress, and inflammation. These processes impair blood vessel function, promote atherosclerosis, and cause damage to nerve tissues, resulting in complications such as cardiovascular disease and neuropathy.
Managing blood glucose levels effectively is crucial in preventing or slowing down these damaging effects.
Diabetes circulatory system & Diabetes circulation symptoms
Diabetes can have significant effects on the circulatory system. It leads to various symptoms:
- Peripheral Artery Disease (PAD): Symptoms include leg pain or cramping during activity, numbness, cold feet, and slow-healing sores.
- Poor Blood Flow: Symptoms may involve tingling, swelling, and changes in skin color in the extremities.
- Heart Disease: Watch for chest pain, shortness of breath, and unusual fatigue.
- High Blood Pressure: Look for headaches, dizziness, and blurred vision.
- Diabetic Foot Problems: Increased risk of infections, foot deformities, and other issues.
Proper management of diabetes, including controlling blood sugar levels and regular medical check-ups, is crucial to mitigate these complications.
Diabetes and Cardiovascular Disease Symptoms
- Diabetes Chest Pain Symptoms: While some may experience chest pain, it is often less pronounced in diabetics. The pain might be more diffuse and less intense than in non-diabetics.
- Type 2 diabetes and heart palpitations: Individuals with diabetes may experience heart palpitations, which can be an indicator of underlying cardiovascular issues.
- Diabetic Heart Attack Symptoms: Look for subtle symptoms such as fatigue, nausea, or shortness of breath, especially if you have diabetes.
Connection Between Type 2 Diabetes and Heart Failure Treatment
The connection between type 2 diabetes and heart failure treatment is significant because both conditions often co-exist, and each can exacerbate the other. Managing one condition effectively can help mitigate the impact on the other.
Managing type 2 diabetes and heart failure effectively requires a comprehensive approach that considers how each condition impacts the other and integrates treatments to address both simultaneously.
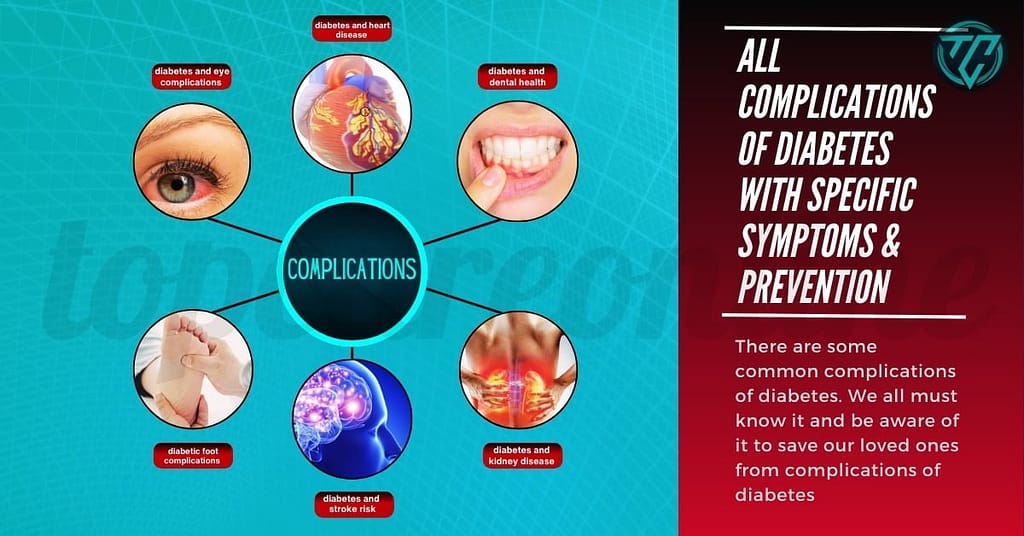
After knowing all these, its quite easy to guess the impact of diabetes with other circulatory complications. Like Cardiovascular Disease, Peripheral Artery Disease (PAD) ,Hypertension (High Blood Pressure) ,Chronic Kidney Disease (Diabetic Nephropathy),Diabetic Retinopathy ,Foot Problems, Cerebrovascular Disease.
Managing Diabetes and Cardiovascular Health
1. Regular Monitoring and Management
To effectively manage the relationship between diabetes and cardiovascular disease, regular monitoring of blood glucose levels is essential. Keeping blood sugar levels within the target range can significantly reduce the risk of developing cardiovascular complications.
2. Lifestyle Modifications
- Diet and Exercise: Adopting a healthy diet and regular exercise routine can help manage blood sugar levels and improve heart health. Foods rich in fiber, lean proteins, and healthy fats, combined with regular physical activity, can have a positive impact on both diabetes and cardiovascular health.
- Medication: Some medications, such as semaglutide, are used to manage type 2 diabetes and may have cardiovascular benefits. However, it’s crucial to be aware of potential side effects, including cardiac concerns.
3. Monitoring Heart Health
Regular check-ups with a healthcare provider are essential to monitor heart health and detect any early signs of cardiovascular issues. This includes checking blood pressure, cholesterol levels, and heart rate.
4. Managing Symptoms
If you experience symptoms such as poor circulation in your feet or hands, it’s important to address them promptly. Diabetes can lead to poor circulation, which may cause complications like diabetic foot ulcers. Strategies to improve circulation include:
- Proper Foot Care: Regularly inspect your feet for any signs of problems and maintain good foot hygiene.
- Medication: Use medications as prescribed to manage symptoms and improve circulation.
Some Common Questions
Is Diabetes Cardiovascular Disease?
Diabetes is not classified as cardiovascular disease (CVD), but it significantly increases the risk of developing CVD. Therefore, while diabetes itself is not CVD, its impact on heart health underscores the importance of proactive management to prevent cardiovascular complications.
Can High Sugar Raise Heart Rate?
Yes, high blood sugar (hyperglycemia) can raise heart rate. Several mechanisms explain this:
- Stress Response: High blood sugar can trigger a stress response in the body. This stress response can activate the sympathetic nervous system, which can increase heart rate.
- Dehydration: Chronic hyperglycemia can lead to increased urination and dehydration. Dehydration can cause an increase in heart rate as the body attempts to maintain adequate blood flow and pressure.
- Electrolyte Imbalances: Elevated blood glucose levels can lead to electrolyte imbalances, such as low potassium, which can affect heart rate.
- Increased Metabolic Demand: High blood sugar levels may increase the body’s metabolic rate, potentially leading to an elevated heart rate as the body works harder to process the excess glucose.
- Autonomic Neuropathy: In people with diabetes, high blood sugar levels can contribute to diabetic autonomic neuropathy, which affects the autonomic nervous system’s ability to regulate heart rate and other functions. This can result in abnormal heart rate responses.
If someone with diabetes experiences a noticeably increased heart rate or other symptoms like dizziness, fatigue, or palpitations during periods of high blood sugar, it’s important to seek medical advice.
What are Semaglutide Cardiac Side Effects?
Semaglutide, a medication used to treat type 2 diabetes and for weight management, has been associated with some cardiac side effects. Here are the key ones:
- Increased Heart Rate: Some patients may experience a noticeable increase in heart rate.
- Heart Failure: There have been reports of worsening heart failure or the development of heart failure, particularly in individuals with pre-existing heart conditions.
- Elevated Blood Pressure: Although not as common, some patients may experience an increase in blood pressure.
- Potential for Fluid Retention: Fluid retention, which can exacerbate heart failure, has been observed in some cases.
Patients with a history of cardiovascular disease or heart failure should discuss potential risks with their healthcare provider before starting semaglutide. Regular monitoring is advised to manage any potential cardiac side effects.
Understanding the relationship between diabetes mellitus cardiovascular disease is vital for effective management and prevention. By staying informed about how diabetes affects heart health, recognizing symptoms of potential complications, and adhering to a healthy lifestyle, you can significantly reduce your risk of cardiovascular issues.