Types | Causes | Symptoms and Diagnosis | Treatment | Preventive Measures |
Foot ulceration is a significant health concern that affects millions of individuals worldwide, particularly those with chronic conditions such as diabetes. These painful sores can lead to severe complications if not managed properly.
What Is Foot Ulceration?
Foot ulceration refers to the formation of open sores or wounds on the foot. These ulcers can occur due to various factors, including prolonged pressure, poor circulation, or underlying health conditions. Foot ulcers can be categorized into several types, with diabetic ulcers being the most common among people with diabetes.
Types of Foot Ulcers
- Diabetic Foot Ulcers: Typically found on the bottom of the foot, these ulcers are a common complication of diabetes, caused by nerve damage and poor circulation.
- Venous Ulcers: Usually located on the lower legs, venous ulcers are often linked to chronic venous insufficiency.
- Arterial Ulcers: These ulcers occur due to poor arterial blood flow and are commonly found on the toes, heels, or lateral side of the foot.
- Pressure Ulcers: Also known as bedsores, these ulcers develop from prolonged pressure on the skin, often affecting individuals with limited mobility.
- Neuropathic Ulcers: These ulcers occur due to loss of sensation in the feet, often seen in diabetic neuropathy, where individuals cannot feel pain or injuries.
Causes of Foot Ulceration
Foot ulceration can be attributed to a range of underlying causes, often involving a combination of factors related to health conditions, lifestyle, and environmental influences. Here’s a detailed look at the primary causes of foot ulceration:
1. Diabetes
Causes:
Neuropathy: High blood sugar levels damage nerves in the feet, leading to a loss of sensation. This makes it difficult for individuals to feel injuries or pressure sores, which can become ulcers.
Poor Circulation: Diabetes can impair blood flow to the extremities, slowing down the healing process and increasing the risk of infections.
Hyperglycemia: Elevated blood glucose levels can affect the skin’s ability to heal and increase susceptibility to infections.
Management:
- Blood Sugar Control: Regular monitoring and management of blood glucose levels.
- Foot Care: Daily inspection of feet and use of proper footwear.
2. Peripheral Artery Disease (PAD)
PAD is a condition where the arteries in the legs are narrowed or blocked, reducing blood flow to the feet.
Causes:
Atherosclerosis: Buildup of plaque in the arteries decreases blood flow.
Reduced Oxygen Supply: Inadequate blood flow leads to decreased oxygen and nutrients reaching the foot tissues, impairing healing.
Management:
- Medication: To improve blood flow and reduce symptoms.
- Lifestyle Changes: Quitting smoking, managing cholesterol levels, and engaging in supervised exercise programs.
3. Poor Footwear
Causes:
Pressure Points: Shoes that do not fit properly can create pressure points on the feet, leading to sores and ulcers.
Friction and Trauma: Shoes that rub or cause friction can damage the skin and lead to ulceration.
Management:
- Proper Fit: Wear well-fitting, supportive shoes with adequate cushioning.
- Orthotics: Use custom insoles or foot pads to reduce pressure and friction.
4. Chronic Venous Insufficiency (CVI)
CVI occurs when the veins in the legs cannot efficiently return blood to the heart, leading to fluid buildup and skin damage.
Causes:
Weak Veins: Malfunctioning valves in the veins cause blood to pool in the lower legs.
Fluid Accumulation: Increased fluid pressure can lead to skin breakdown and ulceration.
Management:
- Compression Therapy: Use compression stockings or bandages to improve venous return.
- Leg Elevation: Keep legs elevated to reduce swelling and improve circulation.
5. Infections
Causes:
Pathogens: Bacteria such as Staphylococcus aureus or Pseudomonas can infect wounds and worsen their condition.
Fungal Infections: Fungal infections can also contribute to foot ulcers, especially in warm, moist environments.
Management:
- Antibiotics: Prescribed to treat bacterial infections.
- Antifungal Treatments: For fungal infections, if present.
6. Trauma and Pressure
Causes:
Repetitive Trauma: Activities or conditions that repeatedly impact certain areas of the foot can lead to ulcers.
Prolonged Pressure: Prolonged periods of sitting or standing, especially with poor cushioning, can create pressure sores.
Management:
- Relief of Pressure: Regularly change positions and use pressure-relief devices like cushions or specialized mattresses.
- Protective Padding: Apply padding to areas prone to pressure or trauma.
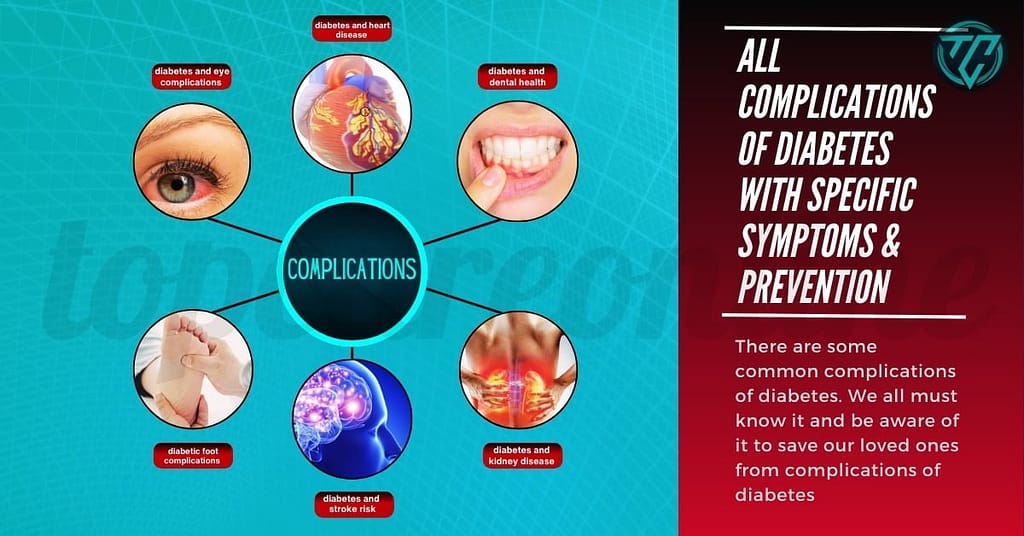
7. Underlying Medical Conditions
Causes:
Autoimmune Diseases: Conditions like rheumatoid arthritis can impair circulation and skin health.
Kidney Disease: Chronic kidney disease can affect fluid balance and circulation, contributing to foot ulcers.
Management:
- Condition Management: Address the underlying medical condition with appropriate treatments and regular monitoring.
- Specialist Care: Consult with specialists for comprehensive management of complex cases.
Symptoms and Diagnosis
Recognizing the symptoms of foot ulceration early is crucial for effective treatment and prevention of complications. Foot ulcers can vary in appearance and severity, and understanding these symptoms can help individuals seek timely medical attention. Here’s a detailed look at the common symptoms associated with foot ulceration:
- Redness
- Overview: Redness around a sore or ulcer is often one of the first signs of inflammation or infection.
- Location: Typically seen around the edges of the ulcer or in the surrounding skin.
- Significance: Redness may indicate irritation, infection, or poor healing.
- Swelling
- Overview: Swelling is a common symptom and can be associated with inflammation or fluid accumulation.
- Location: Usually around the ulcer site or in the surrounding foot area.
- Significance: Swelling can signal infection or a response to pressure and can affect overall healing.
- Pain or Discomfort
- Overview: Pain or discomfort may be present, especially if the ulcer is infected or if pressure is applied.
- Location: Pain can be localized to the ulcer area or radiate to other parts of the foot.
- Significance: The presence of pain can indicate inflammation, infection, or pressure on the ulcer.
- Discoloration
- Overview: Changes in skin color around the ulcer can be a sign of infection or poor blood flow.
- Colors: The skin may appear darker (e.g., purple or black) or lighter (pale).
- Significance: Discoloration can indicate severe tissue damage or necrosis.
- Blisters or Open Sores
- Overview: Initial signs of foot ulceration may include blisters or small open sores.
- Location: Often found on pressure points, such as the soles of the feet or toes.
- Significance: Blisters can rupture and evolve into open sores, leading to deeper ulcers if not treated.
- Drainage
- Overview: Ulcers may produce fluids such as pus, which can indicate an infection.
- Types of Drainage: May include clear fluid, yellowish pus, or a foul-smelling discharge.
- Significance: Presence of drainage is a sign of infection and may require medical intervention.
- Odor
- Overview: A foul odor coming from the ulcer site can be a sign of infection.
- Significance: Odor is often associated with bacterial infections and can indicate the need for urgent treatment.
- Warmth
- Overview: Increased warmth around the ulcer site can be a symptom of inflammation or infection.
- Location: Typically noted around the ulcer or in the surrounding skin.
- Significance: Warmth can indicate an inflammatory response or bacterial growth.
- Reduced Sensation
- Overview: In individuals with neuropathy, reduced or loss of sensation may be present.
- Location: Typically affects the area around the ulcer, making it difficult to feel pain or pressure.
- Significance: Loss of sensation can lead to unnoticed injuries and worsening of ulcers.
- Changes in Skin Texture
- Overview: Changes in skin texture, such as thickening or callusing, can indicate the early stages of ulcer formation.
- Texture Changes: The skin may become rough, hardened, or exhibit abnormal growths.
- Significance: Altered skin texture can be a precursor to ulceration and warrants early intervention.
Diagnosis involves a thorough examination by a healthcare professional. They may use diagnostic tools such as:
- Physical Examination: To assess the size, depth, and severity of the ulcer.
- Wound Cultures: To identify any bacterial infections.
- Imaging Tests: Such as X-rays to check for bone involvement or complications.
Treatment Options
Treating foot ulcers effectively requires a multi-faceted approach. Here are the key strategies:
- Wound Care: Keeping the ulcer clean and protected is crucial. Use appropriate dressings and change them regularly.
- Debridement: Removal of dead or infected tissue helps to promote healing.
- Infection Control: Antibiotics may be prescribed if an infection is present.
- Pressure Relief: Using special footwear or orthotics to reduce pressure on the ulcer.
- Management of Underlying Conditions: For diabetics, controlling blood sugar levels is essential. For vascular issues, medications or surgeries may be necessary.
Preventive Measures
Preventing foot ulcers involves proactive care and lifestyle adjustments. Here are some key preventive strategies:
- Regular Foot Inspections: Check your feet daily for any signs of injury, blisters, or ulcers.
- Proper Footwear: Wear well-fitting, supportive shoes to minimize pressure points.
- Good Hygiene: Keep feet clean and dry to prevent infections.
- Healthy Lifestyle: Maintain a balanced diet, stay hydrated, and engage in regular exercise to improve circulation and overall health.
- Manage Chronic Conditions: Keep chronic conditions like diabetes under control with regular medical check-ups and medication adherence.
When to Seek Medical Help
If you notice any signs of foot ulceration or if an existing ulcer is not healing, seek medical attention promptly. Early intervention can prevent complications and improve outcomes.
Call to Action
If you or someone you know is struggling with foot ulceration, don’t hesitate to reach out to a healthcare professional for personalized advice and treatment. For more information on foot health and managing chronic conditions, explore additional resources and stay updated with the latest medical guidelines.